Sjogren’s syndrome is an autoimmune disorder that affects mucous membranes and associated glands. It is commonly recognized by its characteristic symptoms of dry eyes and mouth. This disease co-occurs with rheumatoid arthritis or lupus.
The disease affects women more than men. It progresses slowly and typical symptoms of dry eyes and mouth may take years to appear after the disease onset.
Symptoms of Sjogren’s Syndrome
Symptoms of Sjogren’s syndrome may vary from person to person and whether it is associated with other autoimmune conditions. It affects systematically and common symptoms include:
- Dry eyes and mouth
- Blurry vision
- Vaginal dryness
- Burning or stinging sensation in the eyes
- Fatigue
- Joint pain
- Skin dryness and rashes
- Cough due to dry nose and mouth.
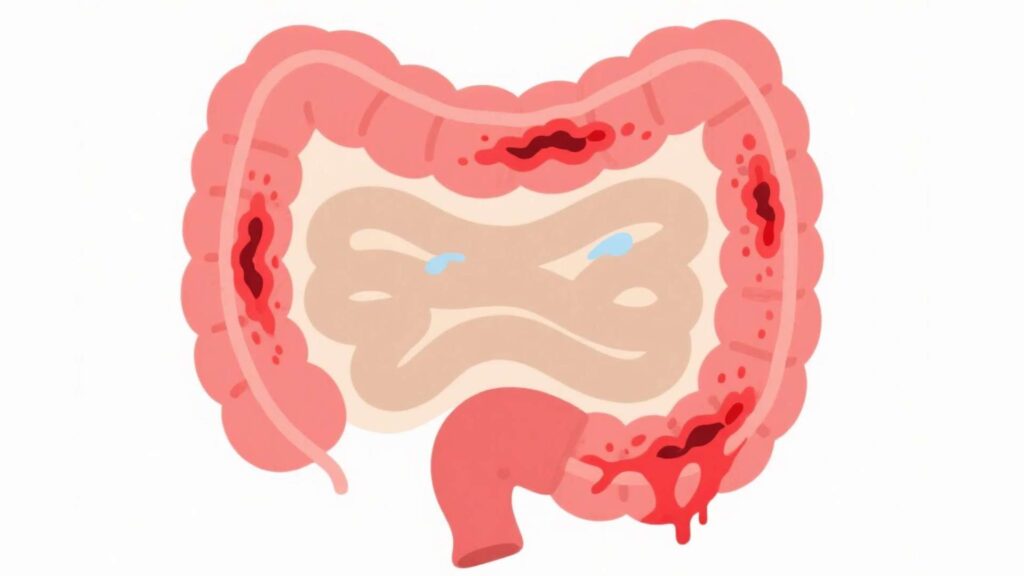
- Inflammation of organs like kidneys. lungs, and pancreas.
- Night sweats and fever.
Sjogren’s Syndrome complications can cause damage to nerves( neuropathy). The symptoms of peripheral nerve damage may include:
- Numbness
- Feeling cold
- Burning sensation (feeling that skin is on fire).
Causes of Sjogren’s Syndrome
Primary Sjogren’s Syndrome (when Sjogren’s Syndrome does not occur with other autoimmune diseases) is an autoimmune condition where the immune system attacks the glands producing secretions like saliva, tears, and mucus. The secondary Sjogren’s Syndrome is triggered by other autoimmune conditions like rheumatoid arthritis and lupus. Common causes include:
- Genetics: Some variants of the HLA gene are risk factors for Sjogren’s Syndrome. Other genes like cytotoxic T-lymphocyte–associated antigen 4 (CTLA4) can also increase the chances of acquiring Sjogren’s Syndrome.
- Viral Infections: Viruses like cytomegalovirus (CMV), hepatitis C, and Epstein-Barr virus can trigger the disease.
- Hormones: Female hormones like estrogen (decreased exposure or lower estrogen levels) can also lead to the development of Sjogren’s Syndrome.
Living with Sjogren’s Syndrome
Sjogren’s syndrome is a lifelong condition with chronic symptoms that can affect social, sexual, and emotional health. To better manage it:
- Keep a journal to monitor the spike in symptoms with weather and food. Avoid immune irritant foods.
- Visit your health provider regularly to monitor the disease progress.
- Avoid stress.
- Educate yourself about the disease and your treatment options.
- Request accommodation and necessary assistance at the workplace.