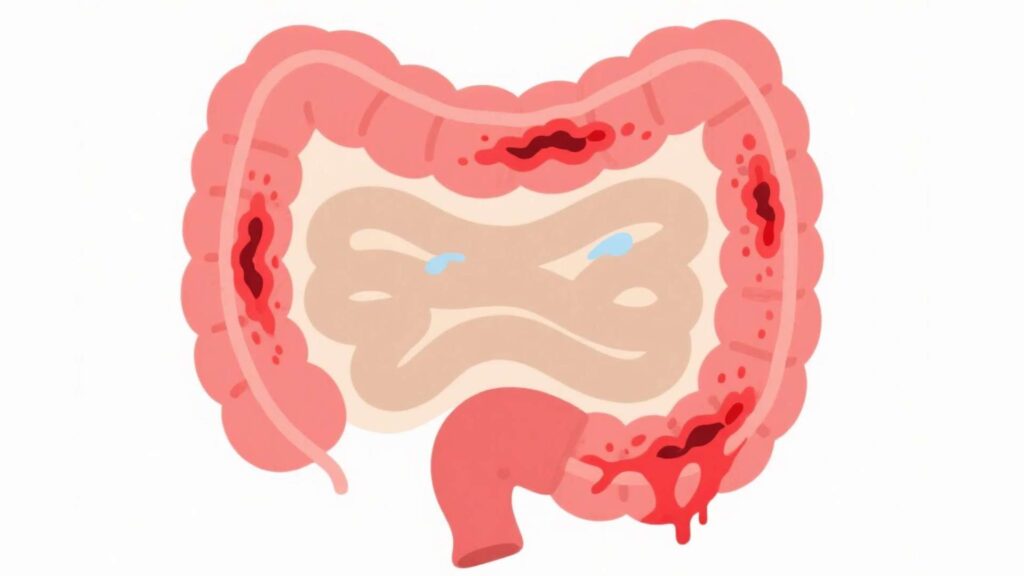
Ulcerative colitis is an inflammatory disease of the large intestine (colon and rectum) that causes irritation and ulcers. It is a chronic disease that develops over time. It is one of the inflammatory bowel diseases (IBDs), the other being Crohn’s disease. It should not be confused with irritable bowel disease.
This disease affects men and women equally. However, people of European descent are at higher risk of getting the disease as compared to Asians.
Types of Ulcerative Colitis
- Pancolitis is a type of ulcerative colitis that affects the entire colon with symptoms of severe diarrhea, abdominal pain and cramps, fatigue, and weight loss.
- Proctosigmoiditis is a type of ulcerative colitis that affects the rectum and sigmoid colon (lower end of the colon) with characteristic symptoms of bloody diarrhea, severe belly cramps, and an urge to poop.
- Acute severe ulcerative colitis affects the entire colon with symptoms of severe bloody diarrhea, fever, and bleeding.
- Ulcerative proctitis is the mildest form of ulcerative colitis that affects the lower part of the rectum (close to the anus). Its common symptom is rectal bleeding.
- Left-sided colitis is an inflammatory disease on the left side of the colon. Its symptoms include cramps on one side of the belly, bloody diarrhea, and weight loss.
Symptoms of Ulcerative Colitis
The symptoms of ulcerative colitis may vary from person to person and type of ulcerative colitis. The common symptoms of ulcerative colitis are:
- Diarrhea and abdominal pain and cramping
- Blood with stool
- Loss of appetite
- Sudden weight loss
- Skin sores and eye pain
- Anemia (too less or deficient RBCs)
- Joint pain
- Always feeling tired
Symptoms can go away (remission) and come back (relapse) without any reason. Keeping a journal of daily routine that flare up the symptoms may help to avoid certain foods, weather conditions, and fatigue that contribute to severe symptoms.
Diagnostic Tests for Ulcerative Colitis
A physician may recommend several tests to confirm that the disease is ulcerative colitis instead of other digestive problems with similar symptoms.
- Blood Analysis: Blood biochemistry for inflammation (ESR and CRP tests) is recommended to assess the activity of the immune system.
- Imaging: Medical imaging of the colon and rectum can be done using X-rays, CT scanning, and MRI scanning. These tests provide overall health of the colon, inflammation, perforations, and other complications.
- Sigmoidoscopy and Colonoscopy: These procedures use a tiny camera attached to a flexible tube. A trained doctor can use sigmoidoscopy to observe the health of the rectum or colonoscopy for the whole colon. A tissue sample (biopsy) can also be taken for analysis and confirmatory test for ulcerative colitis.
- Stool Samples: Stool samples are analyzed for blood, parasites, and worms.
Treatment Options and Disease Management
There is no permanent cure for this condition but there are medicines available to reduce inflammation, manage symptoms, and prevent symptoms flares.
- Aminosalicylates: These are anti-inflammatory drugs that work best in the gut and are often prescribed for ulcerative colitis and Crohn’s disease. These include sulfasalazine (Azulfidine®), mesalamine (Asacol®), etc.
- Steroids: Some symptoms of ulcerative colitis may respond well to corticosteroids like prednisone and budesonide. Steroids have serious side effects and should be taken as advised by your health professional.
- Immune Suppressants: Immune-suppressing medicines work by suppressing the whole immune system. Some of the immune suppressants, called Janus kinase (JAK) inhibitors suppress the enzymes that participate in inflammatory activity.
- Biologics: Biologics are prescribed to subside severe ulcerative colitis. These are antibodies that target the molecules of the immune system like TNF-α that participate in producing inflammation and autoimmune response.
Avoid NSAIDS (ibuprofen, naproxen, etc.) while dealing with ulcerative colitis as these drugs have been found to aggravate the symptoms.
Risks and Complications of Ulcerative Colitis
Most people suffering from ulcerative colitis experience symptoms that come and go, with periods of remission. Severe and chronic ulcerative colitis may produce some complications. While dealing with autoimmune conditions, understanding the potential risks and complications, and taking necessary precautions to reduce the risk is an effective approach to deal with ulcerative colitis.
Bleeding:
Bleeding is a common symptom of ulcerative colitis during flare-ups. Excessive bleeding can lead to anemia, fatigue, and exhaustion. Regular visits to your health provider are also important to monitor ulcerative colitis and overall health. Self-care and adherence to hygiene guidelines as well as treatment plans is an effective way to deal with ulcerative colitis.